by Dr. Iva Lloyd, ND
In times of chaos and change is it always helpful to have an anchor, something that keeps you steady during the storm. Anchors allow us to move forward through times of change by helping us stay grounded and limiting the chance that decisions that we make are based on fear.
The following are some tips on finding an anchor that works for you and supports your health during times of chaotic change.
Analogies
The mind likes analogies as they assist in making sense of chaotic times. They provide a perspective that helps us understand the complexity of new situations that threaten our sense of safety. They assist in providing a sense of order or process during difficult situations. At times, they can also provide a sense of meaning to things that we don't yet understand. For me, the analogies where there is extreme destruction and chaos which result in a "new normal" such as a hurricane, a forest fire, a home renovation or even war, may help explain this current pandemic.
We want to keep in mind that infections that threaten health are not a new thing. Learning from the past can help navigate the current situation. For example, an article in the
European Journal of Cultural Studies has compared the current pandemic to the AIDS crisis 30 years ago in a paper titled, "Pandemic and its metaphors:
Sontag revisited in the COVID-19 era. This article highlights the overwhelming sense of fear that was originally associated with AIDS that has now significantly subsided even though AIDs has not gone away.
Change is Inevitable
Many people handle acute crises quite well. Acute crises, such as accidents, injuries, losing one's job, death of a loved one, the diagnosis of a serious condition and other life events, are seldom welcomed but there is the awareness that "things happen" and you get through them. There is generally a structured process that walks someone through the change. For example, there is a process that you follow once a loved one has passed or if there is a flood in your home - we know what needs to happen and in what order. The sense of structure and process helps us get through significant life events.
Yet, for everyone there is a cap or ceiling on the degree of change that they are comfortable with and that they are able to integrate into their lives and still maintain a sense of being okay. The pandemic is a new type of change for many of us as we are being asked to change because of an invisible external threat. Not to say that there isn't a virus, but the change that has happened as a result has affected people in many different ways.
For some, this pandemic has resulted in the loss of loved ones. For others, it has resulted in concern for their children or their aging relatives or neighbors, the inability to spend time with family and friends and/or the realization of the tremendous mental strain the pandemic has had on people of all ages. For others, it has resulted in the loss of a job or business and/or other financial concerns. And for many, the major impact has been the loss of personal freedoms and civil rights and the impact that this will have on our future.
The factors that have made change difficult for some people to navigate during this pandemic include:
- External Forces: The change has been initiated by external forces in ways that we could never (and still don't) believe were possible.
- Lack of Debate: There has been a lack of consultation, debate and understanding of the broader perspective and breadth of the impact on so many. As Canadians, we are used to filtering out the truth or at least what we believe to be true, through listening to experts debate. During this pandemic there has been pretty much no debate which has intensified the chaos and sense of fear - on all sides.
Acceptance
When there is a significant change that has affected a person's life, it is always helpful to accept the reality of the situation - maybe not initially if there is a chance that things may change back, but eventually. Acceptance is not always about agreement. It is about recognizing that some changes alter the future forever.
With over twenty years in healthcare, I have found that the greatest impact to health is when a person's energy is split - that is, they are living one life yet desiring something else. When your energy is split it drains you, frustrates you and/or it makes you angry. In can also show up in physical symptoms such as pain, inflammation and conditions like autoimmune and others.
This split in energy shows in many different ways. From little things such as eating "clean", but really desiring the junk food you are avoiding. It shows up as choosing a certain job or relationship because they make the most sense, but really desiring something or someone else. There can be a split in energy after an accident or injury when a person doesn't accept that something "bad" happened. At this point in the pandemic, there is a good chance that there will be a split in energy for those that still believe that there is a chance that we will go back to the "old normal".
The aim of acceptance is to make decisions from a point of knowing, not from fear. It is about deciding to move forward within the reality of the new situation versus waiting or wanting things to go back to a previous reality. Knowingness comes from both knowledge and from instinct. For some, knowledge is the most important, while for others it is instinct. Having and trusting both is important.
Avoid Getting Overwhelmed
A little bit of stress and change can be motivating and can help facilitate change. Being overwhelmed, on the other hand, can become paralyzing. It can actually be detrimental to acceptance and can be demotivating. When overwhelmed, the ability to make rationale decisions based on what it best for you is hampered. There is a greater likelihood for people to abdicate their own thinking processes and make decisions out of fear.
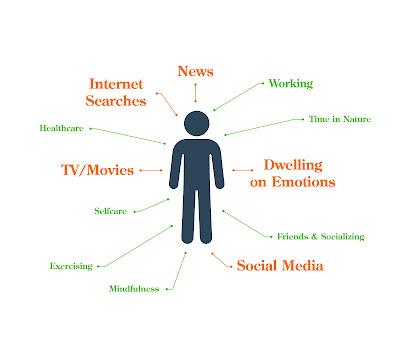
Steps to take to avoid being overwhelmed include:
- Decrease the time you spend listening to or engaged in whatever is overwhelming you.
- Engage in grounding exercises such as going for a walk (ideally in nature or in the forest), gardening, stretching exercises, breathing exercises, etc.
- Choose whole foods and limit sugar, caffeine and processed foods.
- Stay hydrated and active.
- Spend time doing things that you truly enjoy, like listening to music or reading a good book.
- Reach out to others. You may find that a phone call is more nurturing and grounding than text messages (or maybe I'm just showing my age!).
- Remember it is important to have your opinion and beliefs, but it is also important to recognize that others may have a different perspective that warrants consideration.
Truth Versus Relevance
Each person has their own truth, their belief and their position on any specific issue. Linking back to the section on change, we are reminded that the impact of a crisis may vary for different individuals. There is "truth" in many different perspectives - what matters to people is what is relevant to them. We have tended to lose sight of the difference between "truth" and "relevance". For example, the following statements are all "true" (to someone):
- People are dying of infections.
- More people are suffering with mental health issues - young and old.
- The elderly have been more isolated which has had a significant impact on their quality of life and their health.
- The impact on children is immense and may affect them mentally, academically and socially for years to come.
- Our rights and freedoms have been significantly impacted in the last few years.
- Financially we are in trouble in Canada (and many other parts of the world).
- Businesses have closed and are closing all around us.
- Climate change is getting significantly worse and it is being ignored, for the most part.
- Environmental pollutants are likely going to be the next big crisis.
And on and on. Each person has their own "truth" and their sense of "relevance". When in fear, there is a tendency to jump to conclusions based on the truth that is in front of us. When grounded, there is a greater chance on making a decision based on relevance. Relevance takes the "truth" into consideration but it also weighs the short-term against the long-term and weighs a broad range of impacts for individuals and the greater community.
Find Your Lane
An analogy that I use with patients is that life is a paved highway with multiple lanes. When you are in sync with your life you are on the pavement. When you're not, it feels like you are riding on the shoulder and at times it can feel like you are going through life in the ditch. There is choice in life (the different paved lanes), but there is also the need to make choices that are best for you and that keep you on the pavement and not on the shoulder or in the ditch.
"Your lane" refers to what you should be doing. It is about your choices and your role in any situation. For example, as a naturopathic doctor, my "lane" during this pandemic is to provide primary health care by staying current on the research related to post-COVID infections and vaccine-related injuries so that I can support patients in their journey through this chaos.
Each person has the ability to decide what lane they want to choose. An important point to remember is that there are various lanes and a lane is only the "right" lane, when it is aligned with your truth. For some, this pandemic has not changed very much in their life and they are comfortable with the lane they are in. For others, it has felt that they are moving through life in a fog and they aren't sure of their way. They may have lost their business or job and need to find a new way to support their family. Or they may be uncertain of the future for various reasons. Keep in mind, even in war there were those that were fighting the war, those that were building products to support the war, those that were fighting to end the war and those that were just trying to survive the war.
For some, their lane keeps them in the middle of the chaos - and that's okay - if that's their choice. For others, their lane simply involves taking care of a loved one or checking in on neighbors that are alone. Others may be focused on their own personal health, a family crisis or on keeping their job so that they can support themselves and their family. You will know when you are in the right lane as it is easier to move forward, despite the chaos.
Finding Your Anchor
Either at the beginning of the process, or at the end, it is helpful to find an anchor -- or a few anchors. Anchors are things that you can hang onto that pull you through a crisis. Your anchor can be anything that you know to be true - to you. For some, that anchor is family and the desire to spend time with those they love. For others it is astrology and the belief that there is a higher purpose driving this change. For some, it will be the desire to graduate from University and make a difference in the world. Faith or spirituality has been the anchor for some during these uncertain times. For others, it may include another person or practitioner that helps you navigate the change.
An anchor is something outside of the chaos that you know to be true and to be beneficial for you. Your anchor should help provide a perspective that ensures that the decisions that you make are best for you, not only in the present moment, but in the future. Anchors help ensure that we can keep an open mind and make decisions based on relevance to ourselves and others.
Master Your Mind
Is your mind supporting your health and your decision making or is it fighting you? I truly believe that mastering the mind is the key to health in chaotic times and as you get older. The following are some tips on mastering the mind:
- Spend time eavesdropping on your mind. Get a sense for the mind chatter that occupies it.
- The mind generally settles more when it looks at a situation from a number of perspectives. Be open to seeing any chaotic situation from the perspective of you, others, community and global.
- If anxiety, fear, frustration or other emotions are driving your life, then look at ways of quelling these first. Check out books on the topic; talk to friends and family; seek help from your naturopathic doctor or healthcare provider. Reach out.
For further information on the mind, check out the following:
If the chaos in your life is overwhelming you, I recommend that you talk to your naturopathic doctor or other healthcare provider for guidance. You can also call our clinic at 905-940-2727 to book an appointment with
Dr. Iva Lloyd, ND.